Diabetes and Your Eyes: What You Need to Know
People with diabetes have higher than average blood glucose (or blood sugar) levels, which can lead to health problems and eye disease. It is estimated that 10.5% of the adult USA population has diabetes [1]; 24.1% of which have not been diagnosed.
Today, we’re discussing everything you need to know about diabetes and its impact on your eye health.
How can diabetes affect your eyes?
Diabetes can affect your eyes in many ways, making you more prone to certain eye conditions. [2] Some common eye conditions associated with diabetes include:
Diabetic retinopathy
This is a term used to describe retinal disorders that are caused by diabetes.
Symptoms that you may experience if you have diabetic retinopathy include:
- Blurry or distorted vision
- Changes in color vision
- Difficulty seeing at night
- Loss of vision
- Floaters
There are different stages of diabetic retinopathy, based on the presentation and severity of retinal disease. The stages [3] of diabetic retinopathy are:
- Stage 1: Mild non-proliferative diabetic retinopathy
- Stage 2: Moderate non-proliferative diabetic retinopathy
- Stage 3: Severe non-proliferative diabetic retinopathy
- Stage 4: Proliferative diabetic retinopathy
Diabetic retinopathy can also lead to other conditions, such as macular edema. This happens when the macula (where light focuses on the back of your eye) swells due to fluid leaking. Macular edema causes blurry, wavy vision and changes to color perception.
Diabetic retinopathy is irreversible, but treatment can help to stabilize the eye disease and prevent it from worsening.
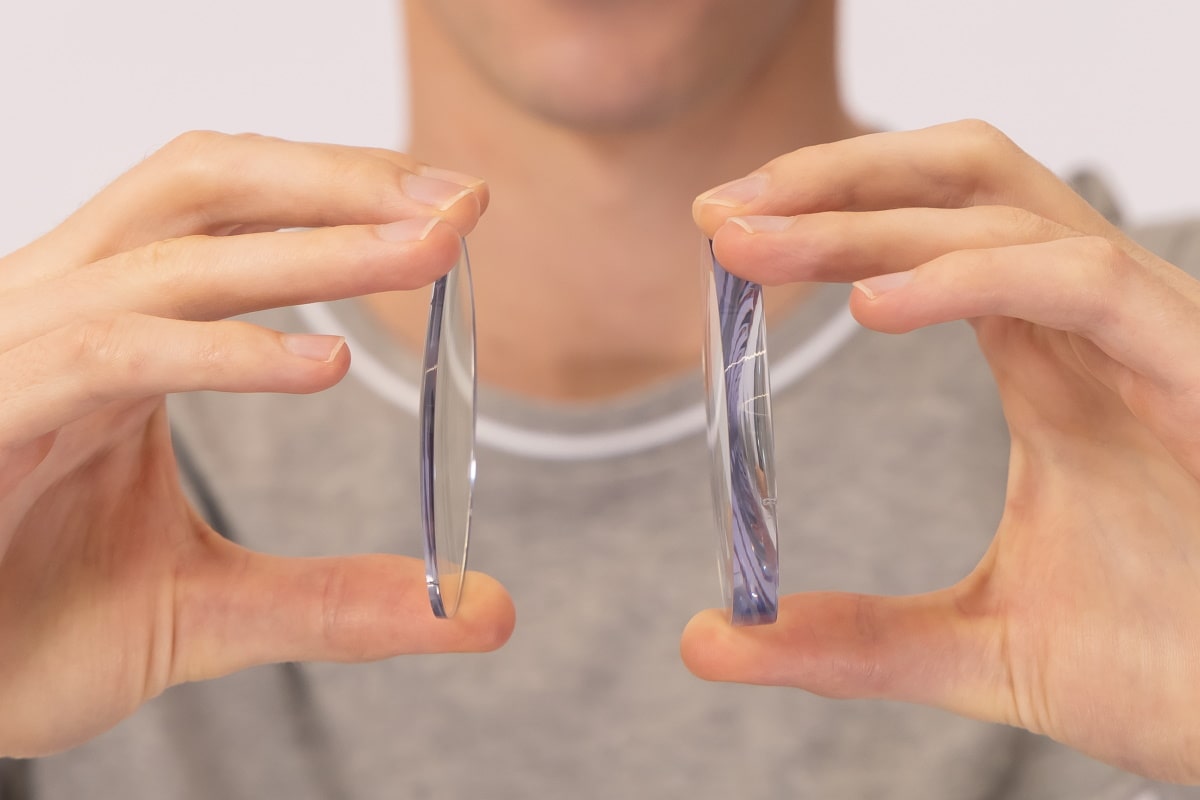
Cataracts
While cataracts are often age-related, people with diabetes often develop cataracts at a much younger age.
Cataracts occur when the lens of the eye becomes cloudy and yellowed. This causes an overall reduction in vision quality. Some other symptoms you may experience if you have cataracts include:
- Cloudy, blurry vision – this will not improve with glasses.
- Sensitivity to bright lights or glare – you may also experience haloes around lights.
- Colors appearing faded or yellowed.
Cataracts can be managed through surgery. This involves the removal of your eye’s natural lens, and its replacement with an artificial lens.
Glaucoma
Glaucoma is an eye disease that causes a progressive loss of peripheral vision. This is caused by damage to the optic nerve (which sends visual information to the brain). Diabetes can increase your risks of optic nerve damage, and in turn your risk of glaucoma.
Symptoms of glaucoma are different depending on the type of glaucoma you have. In early stages of glaucoma, you will often have no symptoms. As the disease becomes more severe you might notice a loss of peripheral vision (this may look like tunnel vision). You may also have blind spots (areas of black in your vision) or blurred vision.
Treatment for glaucoma includes eye drops, laser treatment, or surgery. The type of treatment you receive will depend on the type and severity of your glaucoma. While the vision loss caused by glaucoma cannot be reversed, treatment will prevent you from losing more of your sight.
The connection between diabetes and blurry vision
If you experience blurry vision or any rapid changes to your vision, there is a chance it may be due to diabetes.
Is blurry vision with diabetes temporary?
Fluctuations in blood sugar levels can cause your vision to change. This is because higher levels of blood glucose can cause structures in the eye to change, resulting in changes to your vision.[4]
For example, hyperglycaemia (high blood sugar levels) can cause the lens in your eye to swell. This reduces your ability to focus on things and see clearly. If you experience fluctuating vision, this can be helped by keeping your blood sugar in its target range. This is typically 70-130mg/dL before eating, and less than 180mg/dL within two hours of eating.
Other causes of blurry vision
If you are diabetic, blurry vision is not always caused by fluctuations in blood sugar levels. Some other common causes of blurry vision include:
- Outdated prescription
- Dry eyes
- Cataracts
- Glaucoma
- Age-related macular degeneration
- Eye injury
Who is more likely to develop diabetic eye disease?
All people with diabetes are at risk of developing diabetic eye disease. [5] This includes people with type 1, type 2, and gestational diabetes (diabetes developed during pregnancy).
Unfortunately, your risk of diabetic eye disease also increases over time. The longer you have had diabetes, the more likely you are to develop diabetic eye disease.
You are also more likely to develop diabetic eye disease if you have poorly controlled blood sugar levels.
How do doctors diagnose eye problems from diabetes?
Ophthalmologists and optometrists can screen for and diagnose [4] eye problems related to diabetes by performing comprehensive eye examinations. This will involve looking at the health of the front and back of your eye, as well as measuring your intraocular pressure (the pressure of the fluid in your eye).
They may also take photos of the back of your eyes to monitor for changes over time, and to look at the individual layers of your retina (the back layer of your eye).
If you are diabetic, your eye doctor may also dilate you. This involves putting drops into your eyes that will make your pupils larger. Dilating your eyes will help the ophthalmologist or optometrist to see more of your retina.
The American Diabetes Association offers eye care guidelines [6] for people with diabetes. To appropriately screen for diabetic eye disease, they suggest that patients with diabetes should have dilated, comprehensive eye examinations performed by an ophthalmologist or optometrist. The timeframe for these examinations varies depending on the type of diabetes.
- Adults with type 1 diabetes should have an initial examination within 5 years of diagnosis.
- Patients with type 2 diabetes should have an initial examination at time of diagnosis.
If there is no evidence of diabetic eye disease, your eye doctor will continue to assess you every 1-2 years. If you show signs of diabetic retinopathy, then your eye doctor may choose to see your more often.
How do doctors treat diabetic eye disease?
Treatment for diabetic eye disease varies on which conditions you have and how severe they are. Some common treatments for diabetic eye disease [5] include:
1. Laser treatment
This is used to reduce the leakage of blood vessels in the eye. The two main types of laser treatment are photocoagulation (focal) laser treatment, and panretinal photocoagulation (scatter laser) treatment.
2. Injections
Injecting anti-VEGF into the eye can prevent the formation of new blood vessels forming in your retina. Avoiding new vessel formation is important, as these blood vessels are weak and will leak into your eye. New vessels can cause further eye issues.
3. Surgery
If your diabetes is responding poorly to other treatment, then you may have to undergo eye surgery. Scar tissue from severe diabetic retinopathy can cause the retinal layers to lift and separate (retinal detachment). To prevent this, a vitrectomy can be performed. This is the removal of the transparent gel filling the back of your eye.
What can I do to protect my eyes?
If you have diabetes, there are a number of ways that you can prevent diabetic eye disease. Here are 5 ways [5] you can protect your eyes from diabetic eye disease:
- Have regular dilated eye examinations every 12 months or as recommended by your eye doctor.
- Keep your blood sugar well controlled./li>
- Control your blood pressure and cholesterol levels.
- Eat well and exercise regularly.
- See your eye doctor as soon as possible if you have vision changes or any new symptoms.
What if I already have some vision loss from diabetes?
If you already have some vision loss from diabetes, then you should have this managed by your eye doctor. This may include medications, surgery, or injections. In some cases, diabetes-related vision loss is irreversible. It is most important to focus on preventing your diabetic eye disease from progressing by looking after your overall health.
When should you see a doctor?
You should see a doctor regularly for comprehensive dilated eye examinations. On top of that, if you experience any of the following symptoms, then you should see an eye doctor sooner:
- Changes to your vision
- Eye pain or redness
- Flashes of light or floaters in your vision
- Difficulty seeing at night
- Blind spots or dark spots in your vision
References
- “Diabetes Statistics”, National Institute of Diabetes and Digestive and Kidney Diseases
- “Diabetic Eye Disease”, Centre for Eye Research Australia
- “The 4 Stages of Diabetic Retinopathy”, Healthline
- “Diabetes and Your Eyes”, John Hopkins Medicine
- “Diabetic Retinopathy”, National Eye Institute
- “Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes”, American Diabetes Association

Written by:
Dr. Jordan Marr